The Medicare 8-Minute Rule is a fundamental billing guideline that every rehabilitation professional must understand to ensure proper reimbursement and compliance. Whether you’re practicing physical therapy billing, occupational therapy services, or speech-language pathology, mastering this rule is essential for your practice’s financial health and regulatory compliance.
What Is the Medicare 8-Minute Rule?
At its core, the Medicare 8-Minute Rule determines how therapy providers calculate billable units for time-based CPT codes under Medicare Part B reimbursement. This policy applies specifically to timed procedures—services measured in 15-minute increments—as opposed to untimed procedures like evaluation procedures or re-evaluation billing, which are considered service-based codes billed as single units regardless of time spent.
The rule exists to standardize billing practices across outpatient rehabilitation settings and ensure that Medicare only pays for substantial therapy services actually delivered during direct patient contact.
How the Billable Units Calculation Works
The calculation itself follows a straightforward principle: you can bill one unit of a timed service for every 15 minutes of treatment time. However, the critical element is understanding when you’ve provided enough treatment minutes to justify billing that unit.
Here’s where the “8-minute” threshold comes into play. To bill a single unit, you must provide at least 8 minutes of a timed service. This represents the midpoint rule—the substantial threshold that separates billable from non-billable time.
Breaking Down Treatment Session Duration
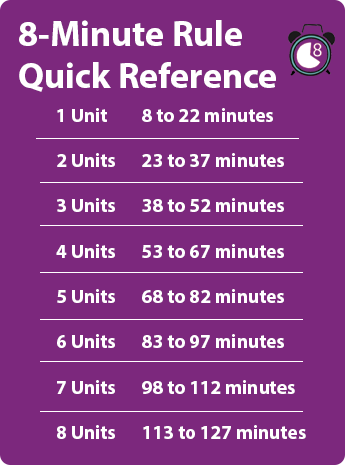
Let’s examine how different treatment minutes translate to billable service units:
8 to 22 minutes = 1 unit 23 to 37 minutes = 2 units 38 to 52 minutes = 3 units 53 to 67 minutes = 4 units 68 to 82 minutes = 5 units
Notice the pattern: each additional unit requires another 15 minutes, but you need at least 8 minutes into that increment to bill it.
Timed vs. Untimed Services
Understanding the distinction between these two categories is crucial for accurate Medicare claims submission.
Timed Procedures Include:
- Therapeutic exercise billing – strengthening and flexibility activities
- Manual therapy techniques – hands-on mobilization and manipulation
- Therapeutic activities – dynamic functional movements
- Neuromuscular reeducation – balance and coordination training
- Gait training procedures – walking and mobility training
These services require documented individual treatment time with the patient, and you must track the exact minutes spent on each activity.
Non-Timed Service Codes Include:
- Initial evaluation procedures
- Re-evaluation billing
- Hot/cold packs
- Electrical stimulation (unattended)
- Mechanical traction
These services are billed as one unit per session, regardless of duration.
Practical Application in Daily Practice
Imagine you’re treating a patient for 45 minutes. During that session, you perform:
- 20 minutes of therapeutic exercise billing
- 15 minutes of manual therapy techniques
- 10 minutes of neuromuscular reeducation
Total timed treatment minutes: 45 minutes
According to the Medicare 8-Minute Rule, 45 minutes falls into the 38-52 minute range, allowing you to bill 3 units total across these timed procedures.
Documentation Requirements and Accurate Time Tracking
The Medicare Administrative Contractor (MAC) takes documentation requirements seriously. Your clinical records must include:
- Start and stop times for each timed service
- Specific minutes spent on each procedure
- Clear description of one-on-one therapy provided
- Patient’s response to treatment
- Clinical reasoning for services provided
Accurate time tracking isn’t optional—it’s mandatory. Any discrepancy between documented time and billed units can trigger audits, denials, or recoupment demands. Clinical documentation improvement should be an ongoing priority in your practice.
Special Considerations for Different Therapy Settings
Concurrent Therapy
When treating two patients simultaneously, you must divide your time appropriately. If you spend 30 minutes with two patients at once, each patient receives credit for 15 minutes of treatment time—not 30 minutes.
Group Therapy Billing
Group therapy billing follows different rules entirely. When treating multiple patients together (typically 2-6 patients) performing the same or similar activities, you use specific group therapy codes. The Medicare 8-Minute Rule doesn’t apply to group sessions, as these are billed per session regardless of duration.
Compliance Guidelines and Common Mistakes
Mistake #1: Rounding Up Too Early
If you provide 7 minutes of therapeutic activities, you cannot bill a unit. You need that full 8-minute substantial threshold. Never round up prematurely.
Mistake #2: Combining Timed and Untimed Incorrectly
Some providers mistakenly include untimed procedures in their total time calculation. Remember: hot packs, unstaffed electrical stimulation, and similar services don’t count toward your timed minutes.
Mistake #3: Poor Documentation
Writing “30 minutes of therapy” without specifying which services were performed and for how long is inadequate. Your documentation must support every billed unit.
Medicare Coverage Policy Updates
Medicare coverage policy evolves, and staying informed is part of professional responsibility. The Medicare fee schedule updates annually, affecting reimbursement rates for both timed and service-based codes. Additionally, modifier usage requirements may change, impacting how you report services.
For instance, the Multiple Procedure Payment Reduction (MPPR) affects payment for outpatient rehabilitation services when multiple procedures are performed on the same day. The highest-valued procedure receives 100% payment, while subsequent procedures receive only 50% payment.
Beyond the Basics: Therapy Cap Exceptions
While therapy cap exceptions have evolved over recent years, understanding annual payment thresholds remains important. When patients exceed certain dollar amounts in therapy services, additional documentation may be required to justify medical necessity.
Your responsibility includes monitoring cumulative therapy costs throughout the year and ensuring that treatment continues to meet medical necessity standards at all times.
Best Practices for Implementation
Create Standard Time-Tracking Systems Implement a consistent method for recording treatment minutes. Whether you use paper forms, electronic systems, or mobile apps, consistency ensures compliance.
Train Your Entire Team Every therapist and assistant in your practice must understand billable units calculation. Regular training sessions prevent costly mistakes.
Audit Your Own Documentation Conduct internal audits quarterly. Review random charts to verify that documentation supports billed units and that the Medicare 8-Minute Rule is applied correctly.
Stay Current on Policy Changes Subscribe to updates from your Medicare Administrative Contractor (MAC) and professional associations. Compliance guidelines change, and ignorance isn’t a defense against audits.
The Financial Impact of Proper Application
Correctly applying the Medicare 8-Minute Rule directly affects your practice’s revenue cycle. Overbilling creates compliance risks and potential fraud allegations. Underbilling leaves money on the table—revenue you’ve legitimately earned but failed to capture.
Consider a practice seeing 50 Medicare patients daily. If each therapist underbills by just one unit per day due to misunderstanding the midpoint rule, that’s potentially thousands of dollars in lost revenue monthly—money that could fund equipment, staff development, or practice expansion.