Medical billing management is the backbone of any successful healthcare practice, serving as the critical link between patient care and financial sustainability. In today’s complex healthcare landscape, efficient billing processes can make the difference between a thriving practice and one struggling to maintain cash flow.
Understanding the Foundation of Healthcare Billing Management
At its core, healthcare billing management encompasses the entire process of submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. This multifaceted system requires precision, expertise, and constant attention to detail to ensure practices receive appropriate compensation for their services.
The journey begins the moment a patient schedules an appointment and continues through treatment, documentation, claim submission, and final payment collection. Each step in this healthcare reimbursement process demands accuracy and compliance with ever-changing regulations.
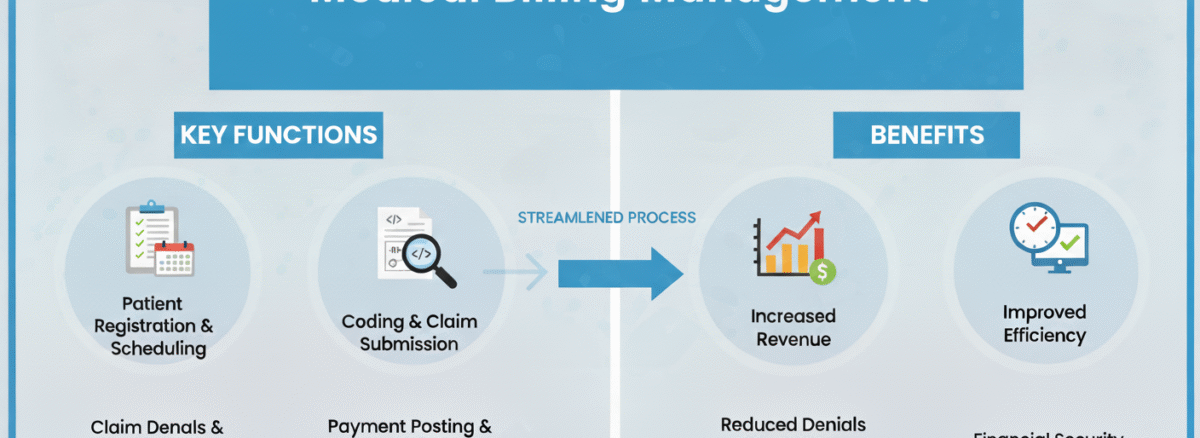
The Critical Components of Medical Billing Management
Revenue Cycle Management (RCM): The Complete Picture
Revenue cycle management (RCM) represents the financial process that healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance. This comprehensive approach ensures that medical billing management operates smoothly from start to finish, minimizing revenue leakage and maximizing collections.
A robust RCM system identifies bottlenecks early, reduces claim denials, and accelerates payment cycles. When properly implemented, it transforms billing from a reactive process into a proactive revenue-generating strategy.
The Medical Billing Process: Step by Step
The medical billing process follows a systematic approach that begins with patient registration and insurance verification. Staff must collect accurate demographic and insurance information, verify coverage eligibility, and determine patient financial responsibility before services are rendered.
After the patient encounter, medical coders translate physician notes and treatment documentation into standardized codes. This billing and coding in healthcare requires specialized knowledge of ICD-10, CPT, and HCPCS coding systems. Accuracy at this stage is paramount—even minor coding errors can result in claim denials or compliance issues.
Medical Claims Management: Ensuring Accuracy and Compliance
Medical claims management involves the preparation, submission, and tracking of insurance claims. This crucial phase of medical billing management requires meticulous attention to detail and thorough knowledge of payer-specific requirements.
Claims must include correct patient information, accurate procedure and diagnosis codes, appropriate modifiers, and supporting documentation when necessary. Clean claims—those submitted without errors—are processed faster and reduce the administrative burden of appeals and resubmissions.
Navigating Insurance Claim Processing Challenges
Insurance claim processing remains one of the most challenging aspects of healthcare revenue management. Each insurance company has unique requirements, varying coverage policies, and different processing timelines. Understanding these nuances is essential for maintaining healthy cash flow.
Common challenges include:
- Pre-authorization requirements that vary by payer and procedure
- Coordination of benefits when patients have multiple insurance policies
- Timely filing limits that differ across insurance companies
- Varying documentation requirements for medical necessity
- Complex appeals processes for denied claims
Successful practices develop standardized workflows that address these challenges while remaining flexible enough to accommodate payer-specific requirements.
Patient Billing Management: Balancing Care and Collections
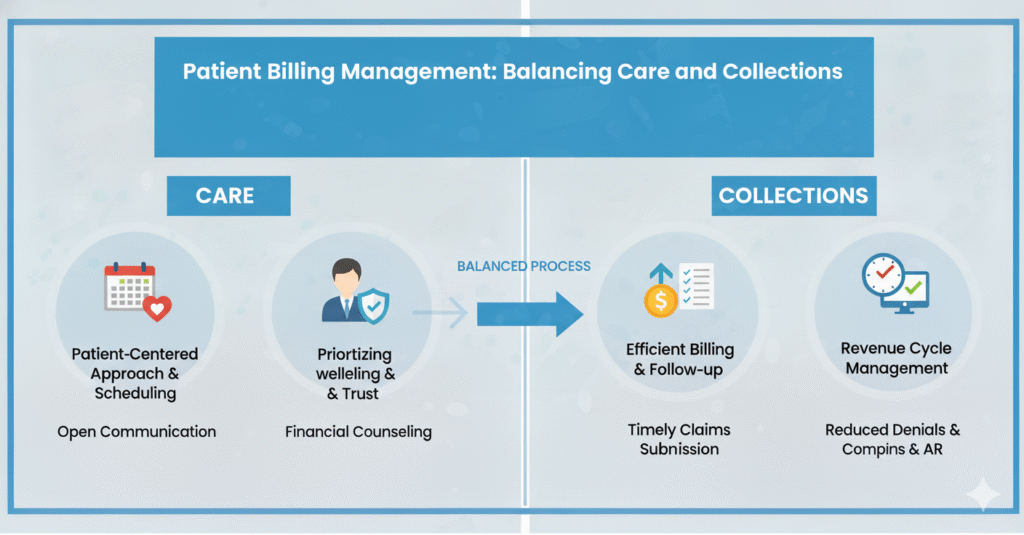
Patient billing management has become increasingly important as high-deductible health plans shift more financial responsibility to patients. Healthcare providers must now function as both caregivers and financial service providers, requiring enhanced communication and payment collection strategies.
Transparent pricing, clear billing statements, and flexible payment options help patients understand their financial obligations while maintaining positive provider-patient relationships. Offering payment plans, accepting multiple payment methods, and providing cost estimates before services can significantly improve collection rates.
Technology’s Role in Modern Medical Billing Management
Advanced practice management systems and specialized billing software have revolutionized medical billing management. These platforms automate routine tasks, flag potential errors before claim submission, and provide real-time analytics on practice financial performance.
Electronic claim submission, automated eligibility verification, and integrated payment posting reduce manual work and minimize errors. Cloud-based solutions offer accessibility and scalability, allowing billing teams to work efficiently regardless of location.
Best Practices for Optimal Healthcare Revenue Management
Implementing best practices in healthcare revenue management requires commitment across the entire organization:
Front-End Excellence: Train front office staff thoroughly in insurance verification and accurate data collection. First impressions matter—errors caught before treatment are far easier to correct than denied claims discovered weeks later.
Coding Accuracy: Invest in ongoing education for coding staff. Regular audits ensure compliance and identify opportunities for improved documentation that supports appropriate reimbursement.
Denial Management: Track denial patterns systematically and address root causes rather than simply resubmitting claims. Analyzing denial trends reveals systemic issues that, once corrected, prevent future revenue loss.
Performance Monitoring: Establish key performance indicators such as days in accounts receivable, clean claim rate, collection rate, and denial rate. Regular monitoring allows for timely intervention when metrics deviate from targets.
Compliance Focus: Stay current with regulatory changes, including updates to coding systems, payer policies, and privacy requirements. Compliance protects practices from audits and penalties while ensuring ethical billing practices.
The Future of Medical Billing Management
Emerging technologies continue to reshape the billing landscape. Artificial intelligence assists with coding accuracy and predicts claim outcomes before submission. Robotic process automation handles repetitive tasks, freeing staff to focus on complex issues requiring human judgment. Predictive analytics identify patients at high risk for payment default, enabling proactive financial counseling.
As healthcare delivery models evolve toward value-based care, medical billing management must adapt accordingly. Success requires not only mastering traditional fee-for-service billing but also understanding quality metrics, bundled payments, and shared savings arrangements.
Transform Your Practice’s Financial Performance
Effective medical billing management is no longer optional—it’s essential for practice survival and growth. The complexity of modern healthcare billing demands expertise, technology, and constant vigilance to achieve optimal financial outcomes.
Ready to Optimize Your Medical Billing Management?
Partner with ZanexMed for Superior Revenue Cycle Performance
ZanexMed specializes in comprehensive medical billing management solutions tailored to your practice’s unique needs. Our team of certified billing specialists and coders brings decades of combined experience in maximizing healthcare revenue while ensuring full compliance.
What ZanexMed Offers:
- End-to-end revenue cycle management services
- Advanced technology platforms for real-time performance tracking
- Dedicated account managers who understand your specialty
- Proven denial prevention and resolution strategies
- Transparent reporting and analytics
- Improved cash flow and reduced days in A/R
Don’t let billing challenges hold your practice back. Contact ZanexMed today to discover how our expertise in medical billing management can transform your revenue cycle and allow you to focus on what matters most—delivering exceptional patient care.
Schedule your free practice assessment now and take the first step toward financial optimization.
What is the difference between medical billing and medical coding?
Medical coding involves translating physician documentation and diagnoses into standardized codes (ICD-10, CPT, HCPCS), while medical billing uses those codes to create and submit claims to insurance companies for payment. Coding comes first in the process, and billing follows to ensure providers receive reimbursement for services rendered.
How long does it typically take to receive payment from insurance companies?
Most insurance companies process clean claims within 14 to 30 days, though timelines vary by payer and claim complexity. Electronic claims typically process faster than paper submissions. Practices can improve payment speed by submitting accurate claims, verifying insurance eligibility beforehand, and following up promptly on outstanding claims.